The Baby Friendly Initiative History
Congratulations Southern California Nurses, for your efforts in promoting the Baby Friendly Initiative.
Hospitals and Maternal-Child Health departments have set a powerful example for women nationwide. To summarize, in 2007 only 29% of USA hospitals used breastfeeding measures. By 2013, this percentage increased to 54%. Additionally, in California, rates increased to as much as 94% for some breastfeeding and 70% for exclusive breastfeeding. Indeed, the attainment of Baby Friendly designation has proven to be a strenuous, but worthwhile journey.
More than one million infants die worldwide every year because they are not breastfed exclusively for 6 months.
If 90% of babies were breastfed exclusively for 6 months, 911 lives could be saved. In addition, $13 billion could be saved in healthcare costs.
What is the Baby Friendly Initiative?
The Baby Friendly Initiative was launched worldwide in 1992 in collaboration with WHO and UNICEF as a quality improvement project. This initiative is a global effort that encourages governments to develop and implement a policy on infant feeding.
To clarify, hospitals who provide a positive environment for breastfeeding receive the coveted Baby Friendly recognition. This process is not easy! Hospitals, must work rigorously to implement strict standards as outlined by the Ten Steps to Successful Breastfeeding. Secondly, healthcare staff must ensure that breastfeeding rates remain above a certain percentage to retain Baby Friendly status. Most notably, the goal is to empower healthcare workers with appropriate education to provide effective breastfeeding counseling.
What does it mean to be a Baby Friendly Hospital?
Baby Friendly designation means that maternal child health departments have successfully implemented the Baby Friendly Initiative’s Ten Steps to Successful Breastfeeding. In short, these steps include: providing appropriate education to enable mothers to make informed decisions about infant nutrition; also, encouraging skin-to-skin immediately following birth; and offering Lactation Specialist services throughout and beyond the hospital stay.
Not only does this initiative help to reestablish optimal infant nutrition, but it has also proven to improve health outcomes in developed countries. In summary, the risks of formula feeding for infants include: an elevated risks of childhood obesity; type 1 and type 2 diabetes; leukemia; and sudden infant death syndrome. Moreover, in women, the lack breastfeeding increases the incidence of: pre-menopausal breast cancer, as well as, ovarian cancer; retained gestational weight gain; type 2 diabetes; myocardial infarction; and metabolic syndrome.
Southern California hospitals who implemented the Baby Friendly Initiative
It is essential for California obstetrical nurses to continue protecting breastfeeding and maternal-child bonding. The percentages of breastfeeding varied among all California hospitals. Below is a summarized list of Southern California hospitals who have: successfully implemented the Baby Friendly Initiative and Ten Steps to Successful Breastfeeding; or, met the Healthy People 2020 Breastfeeding Objectives; including, hospitals who promote the International Code of Marketing of Breast-Milk Substitutes.
California hospital feeding rates are acquired from Genetic Newborn Screenings collected within 24 hours after birth. This data does not accurately reflect ongoing breastfeeding after 24 hours of birth. Alternatively, this data does indeed demonstrate that the proponents of Breastfeeding have been successful in their efforts to communicate the value of Breastfeeding to the community. For more information on breastfeeding rates visit the California’s Department of Public Health website.
Hoag Hospital
Some breastfeeding = 96%
Exclusive breastfeeding = 75%
St. Jude Medical Center
Some breastfeeding = 93%
Exclusive breastfeeding = 63%
St. Joseph Hospital
Some breastfeeding = 94%
Exclusive breastfeeding = 80%
UC Irvine Medical Center
Some breastfeeding = 91%
Exclusive breastfeeding = 70%
Community Hospital of San Bernadino
Some breastfeeding = 90%
Exclusive breastfeeding = 65%
Arrowhead Regional Medical Center
Some breastfeeding = 88%
Exclusive breastfeeding = 77%
Loma Linda University Medical Center
Some breastfeeding = 92%
Exclusive breastfeeding = 71%
Kaiser, San Diego
Some breastfeeding = 97%
Exclusive breastfeeding = 79%
Palomar Medical Center
Some breastfeeding = 96%
Exclusive breastfeeding = 72%
Paradise Valley Hospital
Some breastfeeding = 96%
Exclusive breastfeeding = 72%
Scripps Memorial Hospital, Ecinitas
Some breastfeeding = 97%
Exclusive breastfeeding = 91%
Scripps Memorial Hospital, La Jolla
Some breastfeeding = 98%
Exclusive breastfeeding = 87%
Scripps Mercy Hospital, Chula Visa
Some breastfeeding = 96%
Exclusive breastfeeding = 83%
Scripps Mercy, San Diego
Some breastfeeding = 96%
Exclusive breastfeeding = 85%
Sharp Chula Vista
Some breastfeeding = 95%
Exclusive breastfeeding = 73%
Sharp Grossmont
Some breastfeeding = 94%
Exclusive breastfeeding = 72%
Sharp Mary Birch Hospital
Some breastfeeding = 92%
Exclusive breastfeeding = 81%
Tri-city Medical Center
Some breastfeeding = 96%
Exclusive breastfeeding = 74%
UC San Diego Medical Center
Some breastfeeding = 96%
Exclusive breastfeeding = 75%
The history of breastfeeding
The history of breastfeeding is a fascinating topic. In the beginning breast milk was the only available food for infants. Wet nurses served as alternatives when mothers became ill or passed away. Subsequently, the industrial revolution took place and the need to work caused women to separate from their infants. Wet nurses became a commodity and thus desired or required by many people. As a result, the cost of their services increased. As a matter of fact, early in the 20th century, the attainment of a wet nurse served as a status symbol for the wealthy. For disadvantaged mothers, “dry nurses” irrupted. However, dry nurses often fed newborn infants pablum, an inadequate form of nutrition for infants less than six months of age.
Furthermore, the proliferation of American Hospitals in the late 1800’s to early 1900’s further caused a divide between mothers and their own breast-milk. During this time hospital’s advertised their environment as a safer and cleaner place to deliver infants compared to midwives. Anti-midwife and wet nurse propaganda further antagonized their reputation. Articles and posters such as these left a bad taste in people’s mouths. Consequently, society began to shift away from longstanding maternal care practices. In addition, advances to formula feeding further led to the substitution of artificial feeding. As a result, formula milk became known as scientifically superior to breast milk and formula companies were born.
The Maternalist Movement
The Maternalist movement began with a group of women who wanted to “clean up the environment.” Overall, these reformers encouraged wives and mothers to make the world a safer and cleaner place to live in. Technology provided that possibility in regards to infant nutrition. Well-off mothers could take pride in providing the latest nutritional technology for their babies, whereas underprivileged women could not afford bottles or formula milk. Over time, breastfeeding became associated with uneducated and low income women. On the other hand, formula feeding became affiliated with more civilized, well-off, and conscientious mothers,
Additionally, maternalists were enthusiastic about scheduling. They encouraged women to run their home in a clean, organized manner with a passion for scheduling babies. In fact, their motto was “A good mother is a scheduling mother.” According to the standards of the movement, Breastfeeding was to occur only during certain hours of the day. For example, they encouraged four hours of rest between feedings and not at all during nighttime hours. Lastly, this movement unknowingly supported formula milk by causing lactation insufficiency, therefore prompting mothers to turn to formula feedings.
Formula promotion
In the 1960’s and 1970’s aggressive formula promotion led to wide-spread abandonment of breastfeeding. In addition, companies enlisted hospitals and healthcare professionals to distribute formula by providing free samples. Being that formula was expensive, mothers often diluted the compound to make it last longer. Consequently, many infants died of malnutrition and infections.
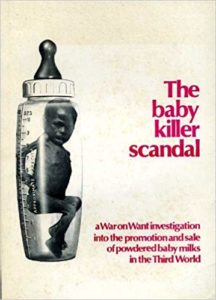
Moreover, the rapid increase of infant mortality rates in 1974 inspired the United Kingdom to publish “The Baby Killer,” which documented the horrific results of formula feeding. In particular, this booklet exhibited graphic images of malnourished infants and starving infants.
Even more, in the past, the United States government went to extreme measures to support formula manufacturers and lobbyists; for the reason that it preserved the US economy.
The national battle between Breast Milk and Formula Milk
Most noteworthy, in response to the associated risks of formula milk the World Health Organization developed the Who Code, also known as International Code of Marketing of Breast-milk Substitutes. To summarize, WHO’s international health policy declares that the advertisement of formula products are unethical and causes harm to infants. Therefore, formula milk sales or free handouts should be legally restricted. Other proposals of the WHO code include:
- Restriction of free formula samples given by the hospitals
- Removal of misleading labels that suggest formula is healthier than breast milk
- Prevention of marketing through healthcare providers that idealize bottle feeding.
Furthermore, the Carter administration, which governed from 1977-1981, was pro-code. In contrast, the Reagan administration opposed the policy due to the fact that it would impact American Corporations. In 1981, under the Reagan administration, the U.S cast the only vote against the WHO code. Formula lobbyists were behind the decision to reject the code. As a result, the U.S. became the leader in restricting formula marketing strategies. During this time Nestle was the largest manufacturer of formula products.
The international battle between Breast Milk and Formula Milk
Each nation had the option to implement or reject The WHO Code. The results were:
- 118 countries adopted the code.
- 3 countries abstained
- 1 country voted against the Code – that was the U.S.
Most notably, the United States government argued the WHO code by using the prospect of antibiotics and clean water supplies to continue making safe and viable formula. The U.S. stands alone as the one modern democracy that has not found a way to reconcile its financial, political, and philosophical concerns. The Code does not restrict manufacturing, sales and use of formula, it is only about marketing. Currently, most nations have legislation to enforce the code, while the U.S. does not. In addition, all major formula companies claim to be Code compliant, but according to a watch dog group (IBFAN), none are.
How formula makers get around the law
Direct marketing through healthcare facilities with free samples is still legal and commonly seen. In actuality, it is not really free. Formula companies simply increase the cost of formula powder to offset the “free samples.” Other examples include:
- Similac sponsors the web site kidsgrowth.com
- Enfamil sponsors WebMD
- Nestle sponsors “World Breastfeeding Week” and all materials are adorned with formula company logos.
- Moreover, when disasters occur the American Red Cross arrives with formula sponsored by companies to save the day.
This cost of formula milk
Formula feeding and all that needs to be purchased can consume 25-50% of the family income. These include:
- The purchase of formula
- The purchase of bottles and nipples
- The healthcare cost of childhood conditions that breast milk could have prevented
- Also, breastfeeding contributes to natural birth spacing which can decrease unwanted pregnancies.
Global strategies to improve breastfeeding rates
The Global Strategy urges that hospital routines and procedures remain fully supportive of the successful initiation and establishment of breastfeeding through the Baby Friendly Initiative. Including:
- Reassessment of Baby Friendly designated facilities.
- Expanding the Baby Friendly Initiative to include clinics, health centers, and pediatric hospitals.
- Furthermore, all governments should develop and implement a comprehensive policy on infant and young child feeding; in the context of national policies for nutrition, child and reproductive health, and poverty reduction.
- All mothers should have access to skilled support to initiate and sustain exclusive breastfeeding for 6 months. In addition, healthcare workers should ensure the timely introduction of adequate and safe complementary foods, certainly, with continued breastfeeding for up to two years or beyond.
- Healthcare workers should be empowered to provide effective feeding counseling. Additionally, their services should be extended in the community by trained lay or peer counselors.
- Also, governments should review progress in national implementation of the International Code of Marketing of Breast Milk Substitutes. Similarly, new legislation or additional measures should be created to protect families from adverse commercial influences.
- Last but not least, governments should enact imaginative legislation protecting the breastfeeding rights of working women, to include, establishing a means for its enforcement in accordance with international labor standards.
So far, the best strategy for improving breastfeeding rates has been the Baby Friendly Initiative.
Although other strategies exist and are effective the Baby Friendly Initiative has been the most successful because its aimed at empowering nurses with education. Hospitals should not mandate that nurses complete courses in Breastfeeding education, rather nurses should motivate themselves to want to learn lactation education. A good nurse is a life long learner who holds a sincere passion for change. In terms of breastfeeding, its time to bring back the Lost Art of holistic maternal child health practices.